Clinical features and diagnostic difficulties
The clinical diagnosis of VWD, particularly type 1, may be a complex task due to the existence of several variables (e.g. blood group, age, sex, exercise, oral contraceptive use) that can influence VWF plasma levels. Substantial variations are often evident during serial sampling of patients suspected of having the disease. About 60% of the variation in VWF plasma levels is due to genetic factors, with ABO group accounting for only about 30%. In type O subjects the VWF level is 25%-35% lower than in non-O individuals. Other unknown genetic factors may also greatly influence VWF levels and, taken together with ABO blood groups and environmental effects, they help to explain the wide variety and incomplete penetrance of type 1 VWD.
It has been proposed several ways of classification because of the wide variability of the VWD, been currently accepted the classification proposed by the Subcommittee of von Willebrand Factor of the International Society of Thrombosis and Haemostasis. This classification distinguished three types of VWD, which correspond with different pathophysiologic mechanisms, clinical patterns and therapeutic requirements, where type 1 (quantitative deficit) is the predominant, type 2 encompasses different qualitative deficits (2A, 2B, 2M and 2N) and type 3 is the total absence of VWF. The diagnosis and classification are based mainly on clinical history and certain laboratory tests as the time of bleeding, the analysis of platelet function overall, the activity of VWF as a Ristocetin cofactor (VWF:CoR), the Ristocetin Induced Platelet Aggregation (RIPA), the antigen quantification (VWF:Ag), the multimeric analysis through low and high resolution gels, etc.
Type 1 von Willebrand disease
Is the mildest and most common form of VWD given that it represents about 80% of all cases. It is characterized by a reduction in mild to moderate levels of plasma VWF: Ag and VWF:CoR. The VWF is normal from a functional point of view, and the plasma levels of Factor VIII (FVIII:C) are reduced in proportion to the level of VWF. The diagnosis for a patient of VWD requires three factors: a significant hemorrhagic history, laboratory results compatible with a VWD type 1 and a positive family history for VWD. Still, the lack of specific symptoms implies, in many cases, a major difficulty to establish a proper and thorough diagnosis.
Its diagnosis is particularly complex because of the presence of multiple variables (blood group, age, sex, contraceptive use) that may influence levels of plasma VWF. About 60% of the variation in these levels of VWF is due to genetic factors, and the ABO group says only about 30% of all of them. In individuals with type O, VWF levels are 25% -35% lower than in individuals not-O. There are other unknown genetic factors that should affect levels of VWF and, together with the blood group and environmental effects, helps to explain the wide range and the incomplete penetrance of VWD type 1.
Type 2 von Willebrand disease
The current classification distinguished four qualitative forms:
Type 2A.
This is the most common among the qualitative variants, with an incidence of 10-15% of all diagnoses of VWD. It is characterized by a loss of the function of VWF platelet dependent due to the absence of forms of high molecular weight protein. Manifests a low ratio of the VWF:CoR and VWF:Ag with the absence of high molecular weight multimers and the disruption of the ability of platelet clumping induced by ristocetin (RIPA).
Type 2B.
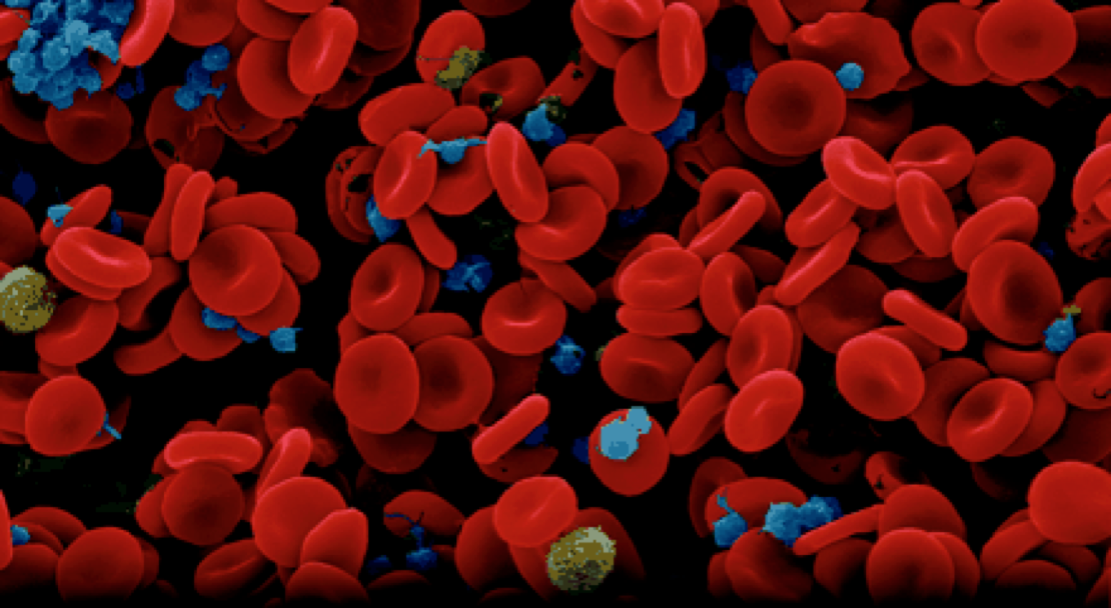
This subtype of VWD represents a gain of function. The disorder is the result of a variety of mutations in the region of union of the glycoprotein Ib, enhancing the capacity of adhesion of VWF in this platelet receptor and causing spontaneous interactions between the VWF and platelets in the bloodstream, a phenomenon that does not happen in the normal VWF. In these patients, there is a link between low VWF: CoR and VWF: Ag as well as an increase of RIPA.
Type 2M.
This subtype is characterized by a decreased RIPA but unlike the type 2A, with the presence of normal multimers in plasma. This differ from type 1 VWD by a low ratio of the VWF:CoR and VWF:Ag.
Type 2N.